Training Module: Prevention of Sexual Abuse and Sexual Misconduct
The protection of the public is of paramount importance to the College. The College emphasizes that the vast majority of its members treat their patients with respect and professionalism; however, the College will work with the public to recognize and address concerns around the power imbalance between health professionals and patients.
The College has created a learning module to address these concerns, accessible to all members through the My CCP portal and to everyone on the College website. This learning module assists members in understanding the definitions of sexual abuse and sexual misconduct within the Health Professions Act (HPA) and the relevant Standards of Practice, as well as the mandatory reporting requirements for regulated members and employers. This module also describes the decision-making guide for compulsory reporting of sexual abuse and sexual misconduct, the College’s complaint and hearing process, the guidelines for maintaining appropriate professional boundaries and available resources. Members can count up to four hours towards a CCP cycle for completing this module.
The module highlights some case studies and the appropriate response. For example, did you know that a sexual relationship between you and your patient constitutes sexual abuse, and that the decision of unprofessional conduct based on sexual abuse means that the Hearing Tribunal must order the permanent cancellation of your practice permit and registration?
For more information, please see the Patient Relations Program page.
Bill 11, Fair Registration Practices Act
On June 19, 2019, the government of Alberta introduced Bill 11, Fair Registration Practices Act. The Act looks to remove entry-to-practice related barriers for internationally educated professionals in Alberta.
The Act will give the Minister of Labour and Immigration the ability to issue compliance orders, request audits on how applications are processed and request reports from the College.
The Fair Registration Practices Code included in the Bill will outline general and specific duties that constitute fair registration, including the provision of information, timely decisions and reasons, internal review processes, assessment of qualification, training, and access to records.
The Bill also establishes a Fair Registration Practices Office. This office will assist the Minister in the exercise of the Minister’s powers and the performance of the Minister’s duties and functions under this Act and the regulations. Click here to read more about this new legislation.
2019 Standards of Practice
The College released its 2019 Standards of Practice on September 1, 2019. The Standards represent the expected minimum level of performance for regulated members and reflect delivery of high-quality, effective, safe, and ethical care to patients.
These Standards are mandatory for all regulated members of the College across all contexts of professional practice.
For more information on the College’s Standards of Practice, please see the Standards of Practice page.
Registered nurses and nurse practitioners prescribing and ordering diagnostic tests
The Government of Alberta has expanded the Nursing practice in Alberta as of May 1, 2019. Registered nurses registered in the College and Association of Registered Nurses of Alberta (CARNA) who meet specific requirements can become authorized to prescribe Schedule 1 drugs (except controlled drugs and substances) and order common diagnostic tests within a particular clinical practice setting.
Before registered nurses can apply for authorization, they must first:
- hold an active permit and be in good standing with CARNA;
- have at least 3,000 clinical practice hours as an RN;
- have at least 750 practice hours in the practice setting/location in which they are seeking authorization to prescribe;
- complete an approved nursing program for prescribing and ordering diagnostic tests;
- have employer support including an employer reference, employer policies, clinical support tools and collaborative practice relationships in the workplace.
A registered nurse practitioner may perform the following restricted activities:
- order or apply any form of ionizing radiation in medical radiography;
- order any form of ionizing radiation in nuclear medicine;
- order non-ionizing radiation in magnetic resonance imaging;
- order or apply non-ionizing radiation in ultrasound imaging, including any application of ultrasound to a fetus.
By Sidsel Pedersen, BRadiog, MRT (R), and Virginia Sanders, MSc, RTR
By Carlos Barrios, MSc, HBSc, RDCS,CRCS, DMS, and Michael Giuffre,BSc, MD
Reprinted with permission from Barrios C and Giuffre M. Adolescent Systemic Hypertension: Late Diagnosis of Coarctation of the Aorta. Canadian Journal of Medical Sonography 2019;10(2):19-22.
Every so often a new therapy shifts the landscape of current practice. It’s a game changer – a disruptive technology. For the past two decades the use of image-guided radiotherapy, using computed tomography (CT), changed the way radiation therapy was delivered to patients with cancer. However, a new technology – magnetic resonance imaging-guided radiotherapy (MRgRT) – is emerging in Canadian practice. Will MRgRT be the game changer CT was?
Radiation therapy is a common treatment for cancer and can be used alone or in combination with chemotherapy and surgery. While CT guided radiotherapy is the current standard of care, a new technology is emerging, and in 2017 the first MRgRT system was approved by Health Canada. MRI may have an advantage over CT guided radiotherapy, as MRI can quickly image soft tissues, which may make it better for visualizing and treating areas that are susceptible to movement in the body (for example movement associated with breathing and bowel motion). Some modalities of MRgRT, such as MR-linac, combine a magnetic resonance imaging (MRI) scanner, which guides the delivery of radiation to the tumour, with a radiotherapy accelerator into one device. The combination of these technologies allows the precise delivery of radiation to the tumour site, while minimizing any potential radiation-related damage to the surrounding tissues. The goal is improved outcomes for patients and health care systems.
To learn more about MRgRT delivery systems, CADTH, which stands for the Canadian Agency for Drugs and Technologies in Health, undertook a Health Technology Update and Rapid Response report (i.e., a rapid evidence review) to see what evidence might be available regarding these technologies. The Health Technology Update, which falls under CADTH’s Horizon Scanning Service, provides brief articles on new and emerging technologies that may be relevant for Canadian health care systems. Our Rapid Response program offers timely evidence reviews to help support health care decision makers.
The Health Technology Update looked at MR-linac systems. At the time of the article (March 2019), there were three facilities in Canada conducting research with MR-linac; one facility in Edmonton, and two facilities in Toronto. The article noted the benefits of using an MR-linac system which can find and treat tumours at the same time. One of these benefits is that if a patient moves during this therapy, even due to normal internal body movement, and the tumour moves out of the field of the targeted radiation, the MR-linac can automatically stop the radiation beam until the tumour moves back into position. And while MR-linac could be used to treat almost any type of cancer, it is anticipated that MR-linac will be initially used for brain, breast, cervix, esophagus, lung, oropharynx, pancreas, prostate, and rectal cancers. However, the CADTH horizon scan also noted the high cost of MR-linac (Canadian costs aren’t known, but in the United Kingdom, installation of MR-linac cost 5.3 million pounds), which may be a barrier to using this type of technology.
It’s also anticipated that MR-linac systems will be operated by a larger team of professionals compared to CT. While CT-guided systems require radiotherapists, due to the novelty of MRI-guided therapies, they will require a team composed of physicians, radiotherapists, medical radiation technologists, and physicists.
In terms of existing research, both the Health Technology Update and Rapid Response noted the lack of research. The Rapid Response report looked for comparative clinical effectiveness (MRgRT systems compared to other image-guided hybrid systems, non-hybrid systems, or before and after treatment comparisons), cost-effectiveness studies, and evidence-based guidelines (full details and questions can be found at: https://www.cadth.ca/magnetic-resonance-imaging-guided-radiotherapy-delivery-systems-cancer-treatment-review-clinical). Only one study was found which compared MRgRT to a linear accelerator system for the treatment of patients with lung cancer. It appeared that there was no difference in lung density between the two systems; however, the study had several limitations and was of low-quality. No cost-effectiveness studies or evidence-based guidelines were found, likely due to the novelty of the therapy. The Rapid Response report concluded that the effectiveness of MRgRT for treating patients with cancer remains uncertain at this time.
What does this all mean for MRI-guided radiotherapy? And specifically, for MR-linac – a new technology, with limited availability in Canada. While it looks like it might be a promising new therapy to treat patients with cancers requiring radiation, it’s still very early days in terms of the evidence for its clinical effectiveness. Only time will tell whether this therapy will replace CT-guided radiation!
- For more information on the Health Technology Update, please visit: https://www.cadth.ca/health-technology-update-issue-23
- For more information on the Rapid Response report, please visit: https://www.cadth.ca/magnetic-resonance-imaging-guided-radiotherapy-delivery-systems-cancer-treatment-review-clinical
- Finally, additional CADTH evidence on medical imaging can be found at: https://cadth.ca/evidence-bundles/evidence-medical-imaging
- And if you would like to learn more about CADTH, visit cadth.ca, follow us on Twitter @CADTH_ACMTS, or speak to Genevieve Chartrand, Liaison Officer for Alberta (GenevieveC@cadth.ca).
The old days of “nose to the grindstone — shoulder to the wheel” are gone. People go to work today with a changed expectation and a changed perception.
All of the research says we are working harder and we will work longer than the previous two generations — the 25-year job ending with retirement and a gold watch is a thing of the past. Given the changing situation, people are looking for work to provide more job satisfaction, enjoyment, interaction, challenge and opportunity to learn and grow. Indeed, people no longer talk about the “job” they want. They talk about the work they want to accomplish and the things they want to learn. They talk about contributions they make and the roles they play in their workplace. Today, we have workers who actively choose the places and times to work and the people to work with. Where people once talked about getting a job, keeping a job and having to work, they now want to talk about being part of a team, sharing responsibilities and accomplishing goals or achieving success. How do we build workplaces to meet these changing expectations?
There are five key elements involved in building a positive, productive workplace:
- Frequent, timely, specific feedback that balances positive and negative information
- Delegation of appropriate responsibility for tasks and outcomes
- Opportunities to work on teams with specific goals and adequate shared information
- Awareness of the big picture and input into the approaches and ways to address challenges, barriers and changes
- Laughter, humour, lightness and fun
Frequent, timely, specific feedback, which balances positive and negative information
The performance appraisal is the formal sharing of feedback based on systems for review and evaluation. It is neither often enough nor specific enough to create a positive, productive workplace. Indeed, many employees leave the performance appraisal interview with comments like:
- “It wouldn’t matter how hard you tried, you would never please her.”
- “I feel like I’ve been watched and every little error was recorded.”
- “You can try hard around here, but you never hear about anything until you mess up.”
The performance appraisal was meant to be a summary of accumulative feedback throughout the year. Instead, it is often the only feedback people receive. In a positive, productive workplace, feedback is given at every opportunity. It is important that feedback be given at an individual level as well as at the team level. Feedback should be balanced. In fact, positive feedback should outweigh negative feedback by a four-to-one ratio. In a positive, productive workplace, people ensure they build a positive foundation, which makes any negative information or criticism more acceptable and understandable. When positive feedback is shared frequently and readily, it opens discussion and creates a solution focus instead of resistance- and problem-focused behaviour. Correction or criticism are then received with the same attitude.
Feedback also needs to be specific and individualized. Lump-sum feedback or team feedback are nice to get; people nod and smile and even comment. However, specific, individualized feedback can motivate productivity and create positive change to a much greater degree. Comments should be directed and timely.
- “You did an excellent job editing the Johnson report. I was impressed with the format changes you made.”
- “Wow — you finished that documentation project two days earlier than anticipated. That must have taken a lot of work and effort.”
- “You really made a lot of progress on that policy manual. There are only six policies left to complete out of sixty. That is excellent work.”
When the feedback applies to specific tasks, people or projects, it is more meaningful and has more power to impact behaviour. Feedback is an essential element for a positive, productive workplace.
Delegation of appropriate responsibility for tasks and outcomes
The definition of delegation changes in a positive, productive workplace. Delegation has often been viewed as getting other people to do things; however, delegation of tasks is now accompanied by shared responsibility. Certainly, people will accept the delegation of a task. The responsibility for completing the task and carrying it through completely builds trust, self-esteem and positive teamwork. When these are in place we begin to see enhanced pride in work well done and increased creativity and innovation.
However, the delegation must be appropriate to the person’s skill development, training, and confidence. When delegation compromises a person’s ability to complete the task with effectiveness and efficiency, it can be overwhelming and frustrating.
Delegation must be accompanied by clear direction, instruction and specific expectations. In a positive, productive workplace, there is no room for assumption, surprises or mistrust. Delegation should always be viewed as a compatibility award for demonstrated capability. Accountability without responsibility places people in a no-win situation.
Opportunity to work on teams with specific goals and adequate shared information
When Abraham Maslow designed his hierarchy of needs, he placed social needs on the third layer of the hierarchy. It followed psychological needs and security needs and preceded ego and status needs. There is now some thought that in a positive, productive workplace, psychological and security needs are often cared for by the system, policies and structure.

Indeed, in a positive, productive workplace, this may be the area in which we can have the most impact. Some researchers say that this has become the foundation of job satisfaction and workplace balance.
When people have the opportunities to work on teams, they are able to address their need to belong and the desire to be in a social environment. Building teams in workplaces becomes an important element for creating a positive place to work.
When people work on teams they also experience the concept of synergy. Synergy is the ability of two or more people to accomplish more and achieve better results than one person working alone. In workplaces where teamwork is the culture, people have the senses of shared responsibility, enhanced communication, increased results and celebration of shared success. These are important to all of us in this fast-paced, dynamic, and challenging era of work.
We have also become aware that working with teams and being on teams is more fun and more interesting in a day-to-day working world.
Awareness of the big picture and input into the approaches and ways to address challenges, barriers and changes
This has been described as an era of inclusion. We used to operate on a basis of “need to know.” We have now added, “want to know.” When people come to work today they want to be informed, updated and aware, and have input on the activities and progress in their workplace. We have a more knowledgeable, curious and interested workforce today. They expect to be respected for their knowledge, experience, and ability to contribute. In a positive, productive workplace, we must make communication the foundation of how we work together. Two-way communication that connects people and their ideas is essential. We must listen, support, and encourage shared information. We have to provide open opportunities and forums for people to share new ideas and discuss ways to improve and enhance our workplaces.
Planning can no longer be done by upper management. Planning must include more people, more input and thus more commitment. Planning activities increase people’s awareness of where we are going, what we are doing, and how we can get there.
When people are aware of the big picture, they are often more interested, they demonstrate more initiative and they look for ways to improve and enhance what they are doing. Knowing how small, day-to-day activities contribute to the overall outcomes and results is empowering and inclusive. The difference is obvious.
Laughter, humour, lightness and fun
A fun-filled workplace is a workplace where people are dedicated and committed to produce quality results. Humour is essential to job satisfaction, teamwork, synergy and everyday involvement. Most people do not head for work in the morning and say, “I can hardly wait to get there — we never have any fun!”
What can you do to initiate laughter? How can you build a lighter, more positive perspective in your workplace? Are you laughing enough?
“You don’t stop laughing because you grow old —
You grow old because you stop laughing.”
— Brenda is a speaker, trainer, writer and consultant. She has been addressing groups for over twenty years on topics related to communications, humour, laughter, positive working skills and wellness in general.
The Competence Committee has completed the 2018/2019 Continuing Competence audit. This year, 8% of the members in the general register were selected for the random audit. Email notification was sent out to these members at the email address they had provided the College during the week of June 4th.
One of the duties of the Competence Committee is to ensure members are compliant with the Continuing Competence Program. Being compliant means that a member must submit a reflective practice review consisting of a self-assessment, a learning plan, and learning activities via the My CCP platform.
Audited members allow the College to access their confidential CCP submissions by pressing a ‘submit’ button. The Director of Education and Competence worked directly with each audited member to provide them feedback and guidance in line with the Committee’s policy to optimize their success on this audit through September.
2018/2019 CCP Audit Information
This year, 197 regulated members (out of a total of 2,463 active members) were randomly audited and the Competence Committee diligently reviewed each submission on October 10 and 11.
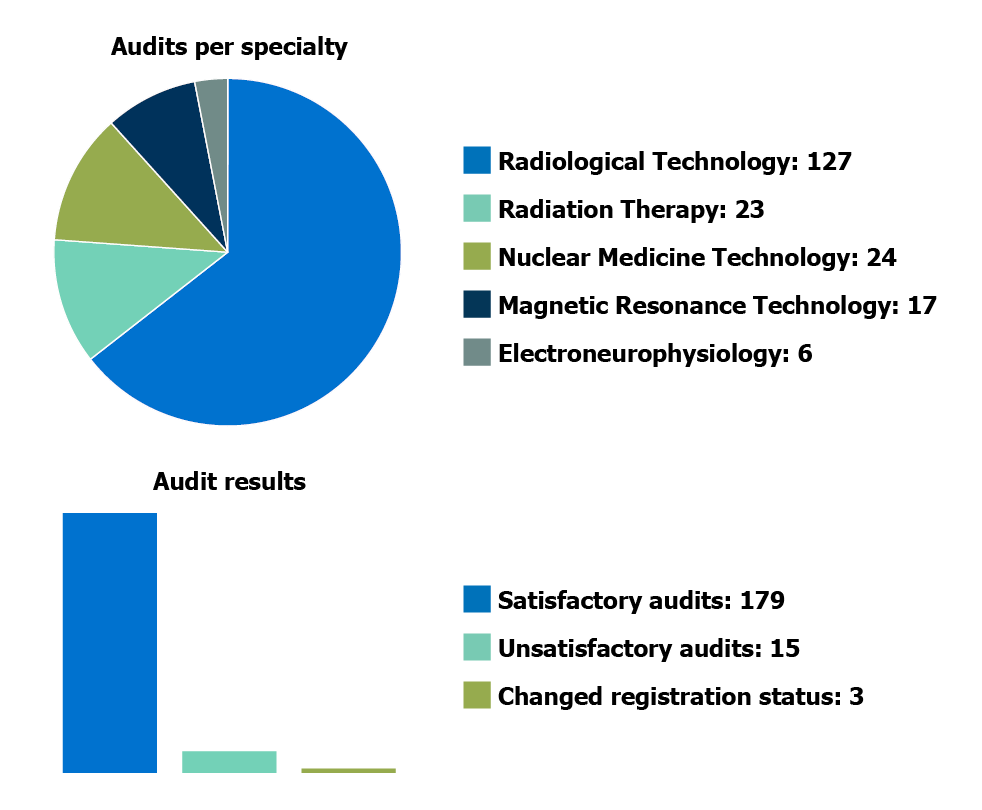
The Competence Committee also conducted a scheduled 5-year review of the Continuing Competence Program on October 9. They received presentations on the continuing competence programs and approach from the College of Medical Radiation Technologists of Ontario and the Alberta College of Combined Laboratory and X-Ray Technologists. Stay tuned for a fuller update on the review in the near future.
Tom, an MR technologist, has been asked by his employer to protocol exams for the MRI department.
Is this activity within Tom’s scope of practice?
According to Alberta legislation, the activity of protocoling MR exams does not require authorization from the College and this activity may be considered appropriate to the technologist’s area of practice.
What training does Tom have to do in order to perform this activity?
A College-approved program is not required as no authorization is needed; it is, however, expected that Tom will have received appropriate training to perform this activity safely, ethically and competently. It is expected that Tom would only protocol exams within his specialty (i.e. an MR technologist would protocol MR exams and a radiological technologist would protocol CT).
Tom should ask himself:
- Does he have the knowledge to perform this competently? For example, consider training in protocoling.
- Does he have the skills to perform this competently? For example, training and familiarity with the procedures being protocoled.
What Standards of Practice apply to this scenario?
As a regulated member of the College, a member needs to practice in compliance with legislation and other documents such as the Standards of Practice and Code of Ethics. The following standards and statements apply to this scenario.
Standard 1.2 Clinical Procedures
To demonstrate this Standard, a regulated member will:
- ensure readiness for the procedure (e.g., confirm type and appropriateness of procedure ordered, ensure requisition contains required information)
- possess the necessary competence to perform the procedure safely, effectively and ethically
- ensure patient safety
- select appropriate equipment and parameters
- identify and communicate with the appropriate healthcare provider any procedural concerns
Standard 2.1 Legislation, Standards and Ethics
To demonstrate this Standard, a regulated member will:
- assume responsibility for the quality and effectiveness of the regulated member’s practice
- maintain and apply the knowledge, skills, judgements and behaviours necessary for competent practice
Standard 2.2 Professional Competence
To demonstrate this Standard, a regulated member will:
- practice within the limits of the regulated member’s competence
- maintain knowledge of current and evolving technologies and integrate new learning into clinical practice as appropriate
Code of Ethics
Principle 1 Responsibility to the public
- Professional judgment
- A regulated member exhibits sound judgement in ensuring that procedures performed are medically appropriate and requested by an appropriately-authorized healthcare provider using consultation as required.
- Council Nominations
- ACMDTT Awards
- Job Postings
- 2020 Membership Meeting
- CONNECT 2020 – Save the Date